There are several possible explanations for why you might not hear well. Here are the four most-common (non-syndromic) reasons for hearing loss, as well as what is typically recommended for them:
1) Sensorineural Hearing Loss (SNHL) and Presbycusis
By far, the most common type of chronic hearing problem in adults is sensorineural hearing loss or SNHL. According to the NIDCD, about 1 in 8 people (13%) in the United States has hearing loss, and men ages 29-69 are almost twice as likely than women to have it. Further, the NIDCD says that 8.5% all adults ages 55-64, one-quarter (25%) percent of those ages 65- 74, and half (50%) of those who are 75 and older have disabling hearing loss. The vast majority of these people have SNHL.
You only have about 12,000 hair cells. These are the tiny filaments inside your cochlea that vibrate and send information to your brain about sound. When they’re gone, they don’t grow back. The most common reason for losing these hair cells is that they gradually wear out over time. This is called age-related hearing loss or presbycusis.
However, presbycusis isn’t a very accurate or scientifically useful term. What we really know to be responsible for presbycusis is the accumulated damage you get from a lifetime of loud noises (ie, long-term noise-induced hearing loss), chemicals and drug exposure (ie, otoxicity that runs the gamut from regular aspirin use to chemotherapy drugs), restricted blood flow to the cochlea (eg, from diabetes, heart disease, etc), and a number of other factors (eg, high fevers, head injury, etc) that can damage or kill those hair cells. The word “sensorineural”, therefore, refers to the loss of sensory nerve receptors inside the cochlea. (Note: There is also the condition called sudden sensorineural hearing loss (SSNHL), which can be thought of as one of the few “emergencies of the ear,” when hearing loss occurs within a relatively short period (3-6 months or less). In this case, you should seek immediate help from a physician.)
Usually in presbycusis, SNHL hearing loss first impacts your hearing in the higher frequencies. That’s the region of sound that contains the consonants—”s”, “t”, “f”, “th”, etc—that are most important for deciphering words. In fact, people with high-frequency hearing loss often complain, “I can hear everything you say, I just can’t understand what you’re saying!” That’s because those consonants are “falling out” of their hearing range. People with SNHL often complain about “listening fatigue” because they have to concentrate much harder to “fill in” those missing speech cues, like a perverse fast-paced game of “Wheel of Fortune.” Some people are really good at this fast-paced game, while others are not. When the listening situation is complicated by competing noise and speech—like that found in bars, restaurants and dinner parties—communication becomes progressively harder and more tiring as the hearing loss becomes more severe.
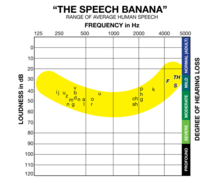
The most common hearing test for assessing hearing loss and SNHL is done with an audiometer—which most people are familiar with from grade school hearing tests where you raise your hand or press a button after you hear a sound. This test yields an audiogram which is a measure of the softest sounds a person can hear at different volume levels and frequencies.
Hearing aids are designed primarily to compensate for SNHL—although the severity of the hearing loss will make a big difference in which type of hearing aid is most effective. Other devices can be helpful in specific situations, including personal sound amplification products (PSAPs) and self-fitting hearing products, and assistive listening devices (ALDs). For example, you might be able to get by with a PSAP or self-fitting hearing aid for a milder hearing loss, but you’ll probably need a professionally fit hearing aid if/when your hearing worsens to a moderate or more serious hearing loss. For very severe and profound SNHL, there are power hearing aids and cochlear implants that work well.
Important counseling on strategies for hearing better (seating in a restaurant, tips of facing a speaker for better lipreading, etc) and auditory training exercises, as well as group aural rehabilitation sessions, may also be offered by a hearing care provider for SNHL. You may also benefit from the experiences and advice of other people with hearing loss by joining organizations like the Hearing Loss Association of America, the AG Bell Association for the Deaf and Hard of Hearing, the American Tinnitus Association, or for cochlear implant users the American Cochlear Implant Alliance, and/or becoming an advocate for better hearing.
2) Conductive Hearing Loss
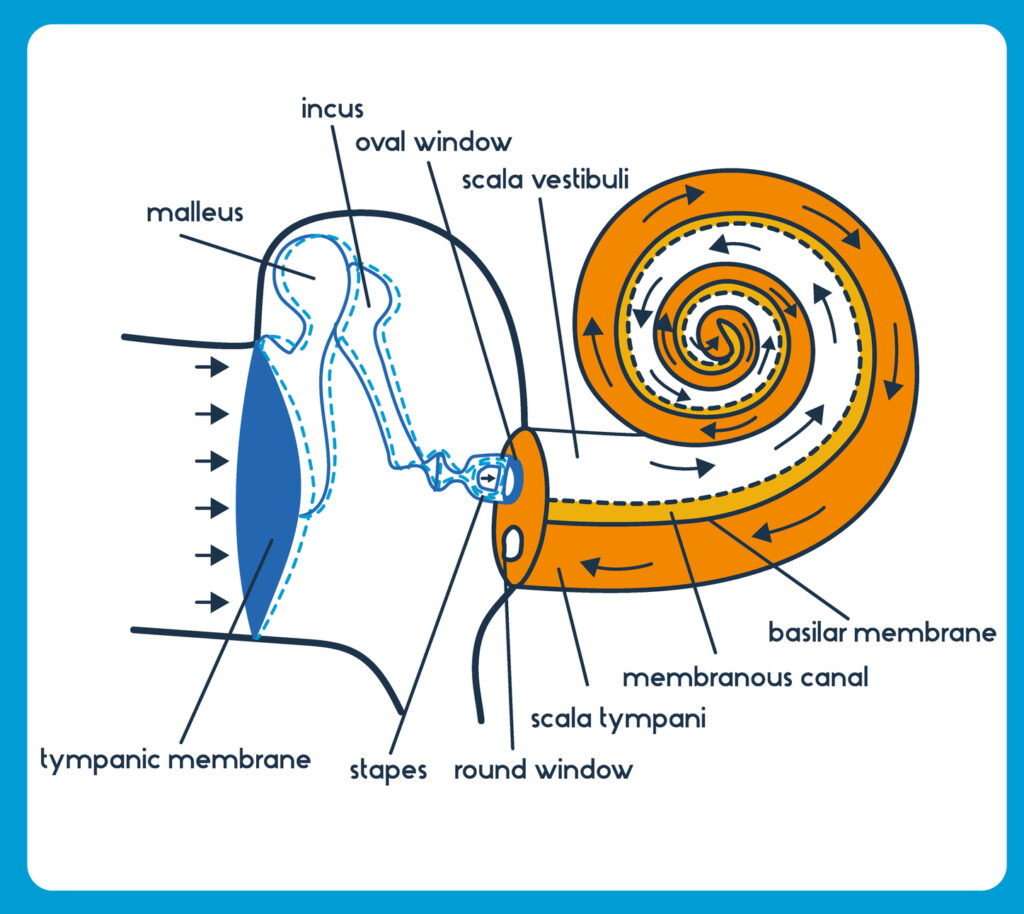
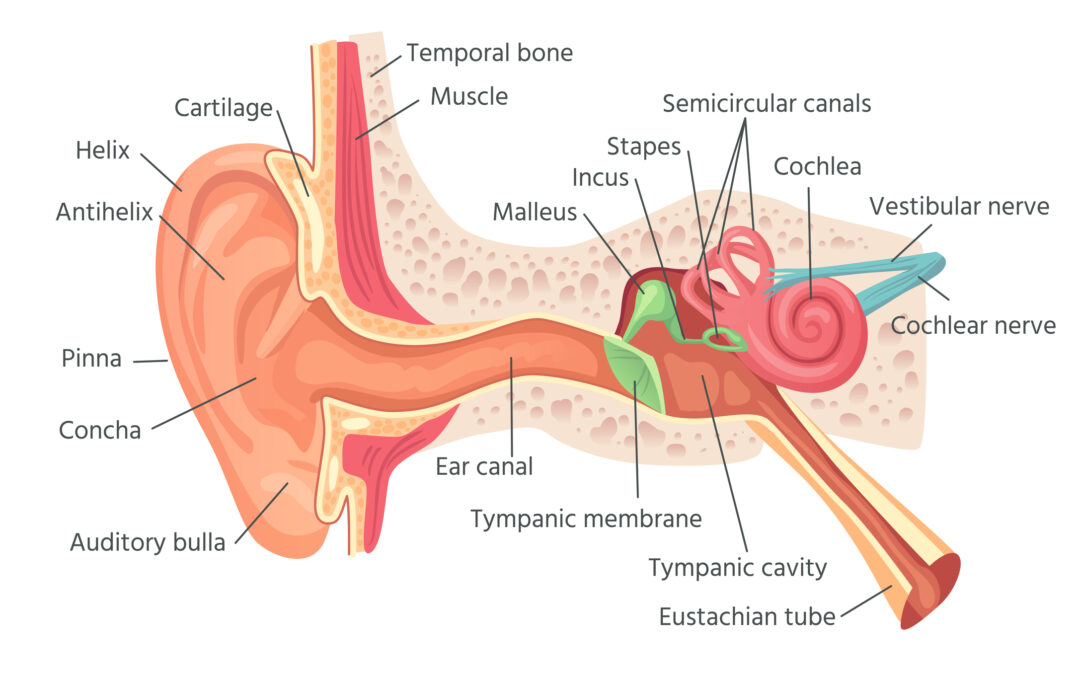
Conductive hearing loss pertains to a hearing loss in your middle ear. If you have a conductive hearing loss, the sound isn’t being properly transmitted from your eardrum, through the tiny bones inside your middle ear, and into the inner ear or cochlea—the organ responsible for “transmitting the sound” into your nerves and sending the auditory signals to your brain. It’s estimated that probably about 5% of hearing losses are due to conductive losses.
A conductive hearing loss can be due to something as simple as a large ball of wax acting like an earplug and blocking sound in your ear canal, to the tiny bones in your middle-ear stiffening (or ossifying) and making it more difficult to transmit the sound to the cochlea. Ear infections (otitis media), frequently seen in children and less common for adults, are another common cause of conductive hearing loss; that’s when fluid builds up inside your middle ear and reduces the efficiency of your eardrum. It’s possible to puncture your eardrum through pressure (eg, deep diving) or by physical perforation (eg, getting too aggressive with a cotton swab). More serious (but rare) medical problems like an acoustic neuroma can also be responsible for a conductive loss—another good reason to see your physician and/or audiologist if you ever experience a hearing loss over a relatively short period of time (eg, 3-6 months). Head trauma, blasts, and other injuries can also disrupt the middle ear and cause a conductive hearing loss.
People with a conductive loss are always examined with an otoscope to see if it might just be ear wax or something else obstructing the ear canal. There are hearing tests, including bone conduction testing (a standard test that involves a small device behind your ear or on your forehead) and tympanometry (a more specialized diagnostic tool), which lend great insights into how the middle ear is performing.
In general, hearing aids can be a good solution for many conductive hearing losses. Additionally, there are bone-conduction hearing aids and bone-anchored hearing solutions (eg, BAHA, Ponto, Bonebridge, or non-implant solutions like TransEar and ADHEAR) which are designed for conductive hearing loss and certain types of single-sided deafness.
3) Mixed Hearing Loss
A mixed hearing loss is usually a combination of SNHL and conductive hearing loss, but can also include APD (see below).
4) Auditory Neuropathy and Auditory Processing Disorders
In addition to SNHL and conductive hearing loss, the auditory nerve fibers that carry the signals from the cochlea to your brain, as well as the auditory cortex itself, can become damaged. The former is usually called auditory neuropathy, whereas the latter is often referred to central auditory processing disorder (CAPD). A blanket term for these hearing problems is auditory processing disorder (APD).
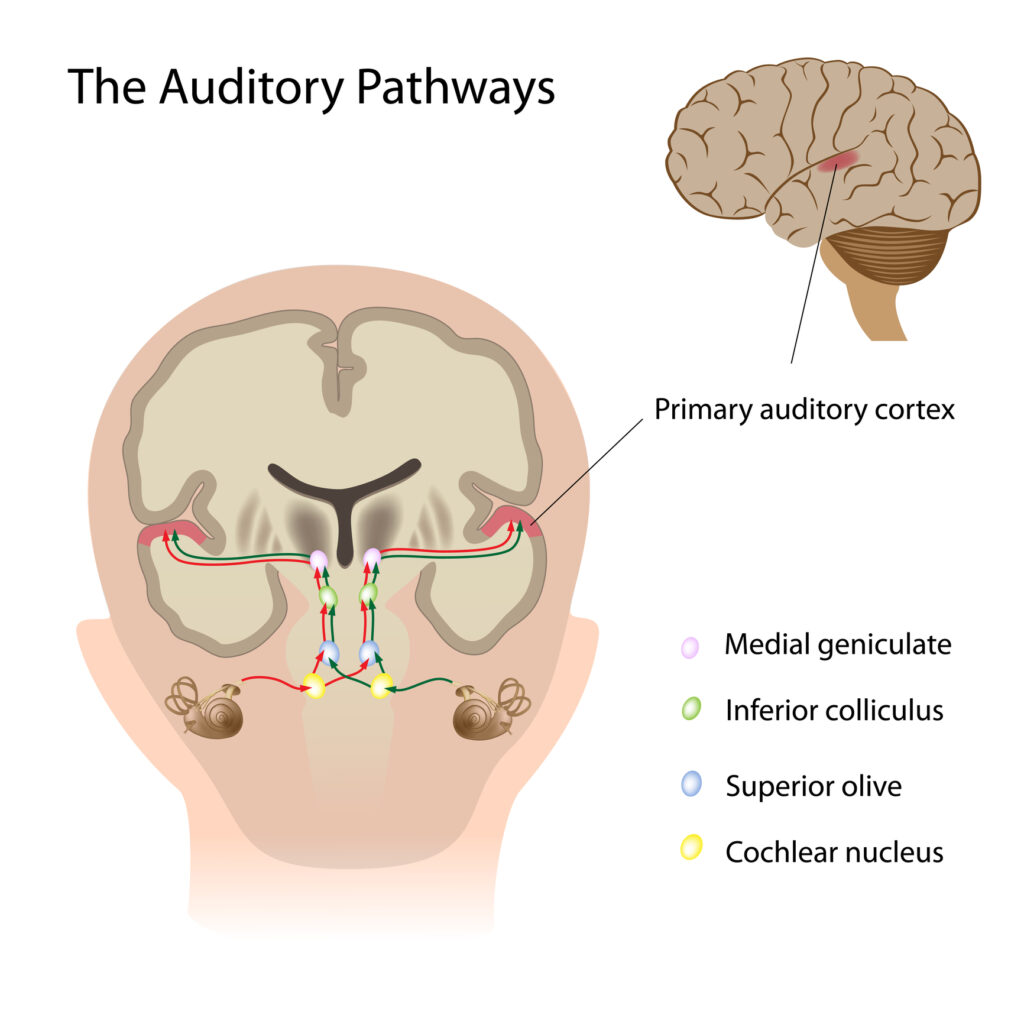
APD and CAPD are probably much rarer as an “sole” cause (as opposed to just a contributor) of hearing loss and communication problems, but they represent an emerging area of auditory science being researched and sometimes hotly debated. In truth, aging and cumulative “wear and tear” on our auditory system probably cause all adults to experience some degree of APD (children can have APD as well, but this website is mostly restricted to issues involving adult hearing loss).
Certain chronic illnesses like diabetes and neurodegenerative diseases (eg, multiple sclerosis, Alzheimers disease), as well as neurotoxins and heavy metals (eg, lead and mercury) have been associated with ADP. Head and blast injuries and longterm hazardous noise exposure without appropriate hearing protection (eg, military vehicles, aircraft carriers, etc) have also been linked to APD.
If warranted, there are diagnostic tests an audiologist can use to find “breaks” or “lesions” in your auditory nerve pathway to the brain or some other “central” problem in your auditory cortex, should this type of hearing loss be suspected. As with any hearing loss, you should immediately see your physician and/or audiologist if you experience a sudden hearing loss or any of the FDA’s 8 red flags, which could indicate a more serious health condition.
In general, recommendations for APD usually involve hearing aids and/or remote microphones or other assistive devices which further help isolate and/or “pull out” the speech elements in communication to enhance listening ability and aid in word understanding. Auditory training exercises may also prove helpful. Ongoing research into treatment pathways for APD continue to be explored.
About the author: Karl Strom is editor of the trade magazine, The Hearing Review, and has been reporting on hearing healthcare issues for over 25 years.
Recent Comments